Overuse of antibiotics in livestock has given rise to drug-resistant germs. Drugmakers say they want to be part of the solution. But a recent campaign urged farmers to administer the drugs to healthy animals daily.
By Danny Hakim and Matt Richtel | June 7, 2019
Facing a surge in drug-resistant infections, the World Health Organization issued a plea to farmers two years ago: “Stop using antibiotics in healthy animals.”
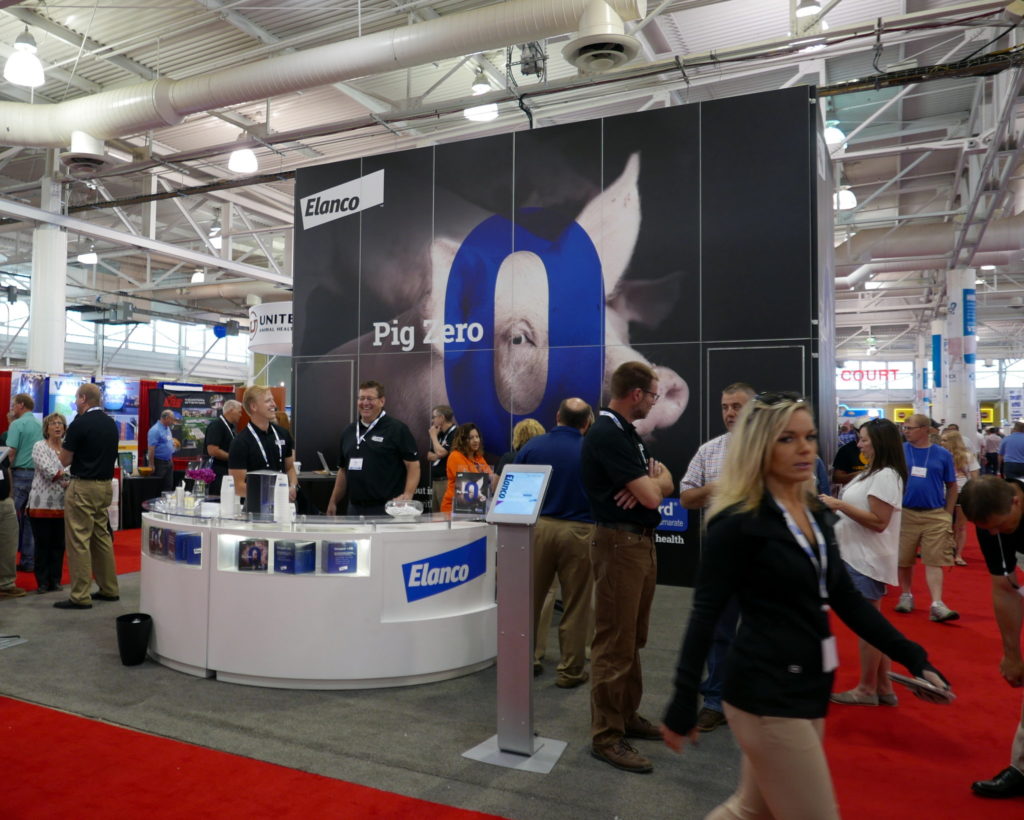
But at last year’s big swine industry trade show, the World Pork Expo in Des Moines, one of the largest manufacturers of drugs for livestock was pushing the opposite message.
“Don’t wait for Pig Zero,” warned a poster featuring a giant picture of a pig peeking through an enormous blue zero, at a booth run by the drugmaker Elanco.
The company’s Pig Zero brochures encouraged farmers to give antibiotics to every pig in their herds rather than waiting to treat a disease outbreak caused by an unknown Patient Zero. It was an appealing pitch for industrial farms, where crowded, germ-prone conditions have led to increasing reliance on drug interventions. The pamphlets also detailed how feeding pigs a daily regimen of two antibiotics would make them fatter and, as any farmer understands, a heavier pig is a more profitable pig.
The rise of drug-resistant germs, caused by overuse of antibiotics, is one of the world’s most nettlesome health predicaments. Excessive use of the medicines has allowed germs to develop defenses against them, rendering a growing number of drugs ineffective for people and animals. The practices of livestock farmers, who for decades have used huge quantities of the drugs deemed important to humans, have long been viewed as one of the roots of the problem, but the role of the companies that make the drugs has received less scrutiny.
Antibiotics continue to be an important part of the business of companies like Elanco, which spun off from Eli Lilly in September, its share price soaring to $33 from $24. While Elanco is developing antibiotic alternatives for animals, like vaccines and enzymes, the antibiotics promoted by the Pig Zero campaign are exactly the kinds that global public health officials are trying to curb. And Elanco is no outlier — its rivals are also urging aggressive use of their own antibiotic cocktails.
“The reality is that antibiotics and large-scale industrial farming really grew up together,” said Dr. Gail Hansen, a former state epidemiologist and state public health veterinarian in Kansas, who sits on advisory boards addressing antibiotic resistance. She equated the problem with climate change. “By the time people understand and believe it,” Dr. Hansen said, “it may be too late.”
Elanco had already been put on notice about the drugs used in its Pig Zero push. In 2015, the Food and Drug Administration warned Novartis Animal Health, which had been acquired by Elanco, that the same antibiotic cocktail was “unsafe” and “misbranded,” because it was being illegally marketed to fatten pigs, rather than to simply treat disease. One of the drugs, tiamulin, has been a top seller for Elanco; the W.H.O. views it as medically important to humans, but American regulators do not. Pig Zero trumpets the benefits of coupling tiamulin with chlortetracycline, a drug made by Elanco’s competitors that both American and international regulators consider medically important to humans.
In an interview at Elanco’s headquarters outside Indianapolis, Jeffrey Simmons, the chief executive, said the company had decided to change the program’s marketing and to stop distributing the Pig Zero brochure after The New York Times began asking questions about it.
“We’re trying to be stewards and leaders at the same time,” said Mr. Simmons, adding that the brochure “wasn’t misrepresentation, necessarily, relative to the label or the science, or how a farmer would look at it.”
Dr. Shabbir Simjee, Elanco’s chief medical officer, said drugs like those in the campaign “would never be administered” in a herd “without some animals being physically sick,” adding that “there would need to be some animals showing clinical signs.”
He likened treating a herd to caring for children in a nursery: “If one child gets sniffles, you usually find that the whole class ends up with a cold, and this is exactly the same principle.”
But children almost certainly would not all be treated with preventive antibiotics in such a situation, and many scientists believe animals often should not be treated that way, either.
The connection of overuse of antibiotics in livestock to human health takes two paths: As bacteria develop defenses against drugs widely used in animals, those defense mechanisms can spread to other bacteria that infect humans; and, resistant germs are transmitted from livestock to humans — through undercooked meat, farm-animal feces seeping into waterways, waste lagoons that overflow after natural disasters like Hurricane Florence, or when farm workers and others come into contact with animals.
New F.D.A. regulations put in effect in the waning days of the Obama administration prohibited farms from fattening livestock by lacing their feed with medically important antibiotics. The new rules, along with rising consumer demand for antibiotic-free meat, cut antibiotic use significantly in 2017. But such drugs are still routinely given to pigs and cattle, accounting for almost 80 percent of medically important livestock antibiotics in the United States and nearly 5,000 tons of active ingredient. Worldwide use is projected to keep rising sharply as growing middle classes in places like China and Brazil demand more meat.
Ellen Silbergeld, a professor at Johns Hopkins University, who has worked with the W.H.O. on drug resistance, called the continuing promotion of the drugs by pharmaceutical companies “very dangerous.”
“The reason they’re doing it, though, is money, honey,” she added. “That’s what it’s all about. That’s what it’s always been about.”
Now, the industry has an important ally in Washington: President Trump, who appointed one of Elanco’s former executives, Ted McKinney, as under secretary of agriculture for trade and foreign agricultural affairs. Mr. McKinney told international food safety regulators at a meeting last summer in Rome that they were too singularly focused on consumers, at the expense of pharmaceutical companies and research scientists working to meet growing global demand for food. “We have got to rededicate a focus on them as our customers,” he said.
‘Purpose-driven leader’

In 2015, Mr. Simmons, Elanco’s chief executive, joined a White House summit meeting to pledge the company’s commitment to curbing antibiotic use.
Sylvia M. Burwell, then the health and human services secretary, hailed the gathering as a “hopefully historic step to protect the health of our nation.” Dr. Thomas R. Frieden, the director of the Centers for Disease Control and Prevention at the time, warned that antibiotic resistance “could result in the medicine chest being empty when we need it most.”
Mr. Simmons outlined Elanco’s lofty aims. “We’re going to create antibiotic alternatives,” he said, adding, “We believe strongly that there are solutions, there are pipelines, there are options.”
A farm boy from upstate New York, he was a nearly 30-year veteran of Eli Lilly when Elanco spun off last year with its 5,800 employees. His wife helps run a church food bank. Mr. Simmons sits in an unassuming cubicle on Elanco’s campus.
He refers to himself as a “purpose-driven leader” on a mission to fight hunger — echoing the megachurch founder Rick Warren’s best-selling book “The Purpose-Driven Life,” which Mr. Simmons has read and taken to heart. He uses social media to spread a sort of protein-affordability gospel: “#Protein is a nutritious part of a balanced diet, but many don’t have access to it,” he once wrote on Twitter. “We can/must change this!”
While microbiologists emphasize the urgency of fighting antibiotic resistance, agrochemical industry veterans like Mr. Simmons say it must be balanced against hunger and the world’s growing demand for food. He often recounts his time as an executive in Brazil, when an anguished guard in his gated community sought help feeding his two children.
“I’m not doing it for a paycheck or profits,” Mr. Simmons said in an interview. “Purpose has to override that.”
(He does get a paycheck, though. His total compensation was $5.4 million last year.)
Financial disclosures for Elanco and its rival Zoetis, which spun off from Pfizer in 2013, show the two companies sell roughly $2 billion annually in livestock antibiotics. In Elanco’s case, antibiotic sales represent more than one-third of its overall business. Some antibiotics, like monensin, a top seller for Elanco, belong to a class not used in people, and thus are not considered a resistance threat. But so-called shared-class antibiotics, like chlortetracycline, are used in humans and animals, creating risk for resistant infections.
Mr. Simmons said that while Elanco “started as an antibiotic company,” antibiotics that are medically important for people and used in livestock feed now make up only 5 percent of its sales. “We’re not building our company on that 5 percent,” he said. But the company has also said that 12 percent of Elanco’s sales overall, including antibiotics used in feed and administered in other ways, come from medically important antibiotics.
While consumer demand has made developing alternatives an industry imperative, few companies are eager to cede ground on existing business.
Del Holzer, who was the director of meat and poultry for Elanco’s global industry food team from 2012 to 2017, said the company and its competitors want to take positive steps and look good, to a point.
“They want to do the right thing,” said Mr. Holzer, who now works for a division of the agriculture giant Cargill, an Elanco competitor that develops antibiotic alternatives. “But they say, ‘My bottom line is my shareholders will be really pissed at me.’”
An antibiotic boom

When antibiotics were first discovered more than a century ago, no one intended them for animals. But then an American company, Lederle Laboratories, announced in 1950 that chickens grew faster when they were fed chlortetracycline, one of the drugs included in the Pig Zero campaign.
By the early 1960s, almost half of livestock antibiotics were aimed at making animals fatter. Drugs were marketed by the barrel; a 50-pound chlortetracycline bag advertised in 1972 in The Herald, in Jasper, Ind., cost $9.25.
A Purina Pig Chow ad that appeared in an Iowa newspaper in the early 1960s promised that it was “power packed with the potent vitamins, minerals and anti-biotics pigs need for fast growth and good health.” Another ad, in a Missouri paper, promoted “full-o-pep Pig Grower,” a feed laced with antibiotics.
Yet scientists already had misgivings. In 1969, the Swann Committee report, commissioned by the British Parliament, concluded the problem of antibiotic resistance was significant. In 1976, a landmark study published in Nature found that resistant E. coli strains could be passed from chickens fed with antibiotics to other chickens, and then to farm workers.
“It was pretty obvious to me that the prudent thing to do would be to take low levels of antibiotics out of animal feed,” said Dr. Hansen, the former state epidemiologist in Kansas. As an F.D.A. employee in 1978, she gathered evidence for Congress linking antibiotic use in livestock to resistant infections in humans, but no action was taken.
“The science was there, the evidence was pretty easy,” she said. “It was a slam dunk.”
The pharmaceutical industry has pushed back. In 1997, researchers from Elanco were among those who authored a lengthy review in the Journal of Applied Microbiology dismissing concerns about antibiotic use in animals, writing, “We are confronted by a lack of information, a wall of ignorance.”
Pharma companies kept a stranglehold on basic information. Various estimates by academics and public policy groups claim as much as 80 percent of American antibiotic sales go to livestock. But the industry has assailed such projections, calling some “agenda-driven junk science,” while simultaneously lobbying to block legislation requiring more disclosure of antibiotic use.
Mr. Simmons of Elanco has long played down livestock’s role in spreading resistant microbes to humans.
“The most serious pathogens are not related to antibiotics used in food animals,” he said. “Of the 18 major antibiotic-resistant threats that the C.D.C. tracks, only two, campylobacter and nontyphoidal salmonella, are associated with animals.”
But such oft-repeated statements, made even in Elanco’s securities filings, refer only to food-borne strains like antibiotic-resistant salmonella that can be found in raw chicken, for example, while ignoring the myriad ways pathogens can be transferred.
There is a growing body of research establishing links between Clostridium difficile, or C. diff, in livestock and humans, viewed by the C.D.C. as an urgent threat. Broad-spectrum antibiotics in livestock provide “a survival advantage to antibiotic-resistant C. difficile strains,”according to a 2018 study by Australian researchers. Similar studies exist for E. coli and methicillin-resistant Staphylococcus aureus, known as MRSA — the C.D.C. even lists different animals like cows, goats, sheep and deer that can pass E. coli to humans.
“We’ve seen antibiotic-resistant bacteria that can leak into the environment through water and dust, jump to the skin of farmers and swap genes with other bacteria,” said Sarah Sorscher, deputy director of Regulatory Affairs at the Center for Science in the Public Interest, an advocacy group. “And that’s still just scratching the surface on the science. By the time we understand the full magnitude of this threat, it may be too late.”
There has been progress. In 2017, when the F.D.A. effectively banned the use of medically important antibiotics to fatten livestock, their consumption fell by a third that year.
But health experts say the regulations did not go far enough and see a sleight of hand at work, with industry marketing now presenting routine antibiotic use as a “proactive” necessity and weight gain an ancillary benefit, as Elanco did in the Pig Zero marketing campaign.
Before her death last year, Representative Louise M. Slaughter, a New York Democrat who was the only microbiologist serving in Congress, lamented the F.D.A.’s new rules as being riddled with loopholes.
“It’s useless,” she said of the regulations. “That’s why the industry’s supporting it.”
A move to alternatives

A recent tour of Elanco’s labs at its Indiana headquarters swept past a virology lab and a large machine analyzing the DNA of thousands of hamster cells. Amid beakers and hardware, scientists in coats and protective glasses discussed their efforts to find alternatives to antibiotics.
Aaron Schacht, Elanco’s head of research and development, said those alternatives could include enhancing the animals’ own immune function, immunizing them against particular pathogens or reshaping their gut bacteria to favor the good ones.
“Could we eliminate the need for broad-spectrum antibiotics? I think it’s possible,” he said. “Now let’s let the science play out.”
But change comes in fits and starts. Mr. Holzer, the former Elanco official, said the drugmaker had created “country-specific websites” where “there were certain things you couldn’t talk about in the U.S., but then talk about in Poland.”
“It’s a bit of a hypocritical thing,” he added. “Elanco wants to lead the charge on antibiotic use but then sells into these countries that could become the biggest part of the problem. The idea is that as long as we don’t lose antibiotics in country XYZ, we can take our hit in the U.S., and get the P.R. for it.”
Elanco called Mr. Holzer’s comments “completely inaccurate.” Colleen Dekker, a spokeswoman, said the company no longer included “growth promotion” — fattening up animals — as an approved use for medically important antibiotics worldwide, “regardless of what local regulations allow.” The company was also intentionally decreasing its sales of such drugs, she said, showing that “this is far more than a ‘P.R. effort.’”







Aaagh. Hasn’t it been over a decade that we’ve been reading about the dangers of anti-biotic resistance and aren’t over 80% of antibiotics given to animals, especially those in CAFOs! How can we be so short sighted! I dread visiting friends in the hospital with the warnings about MERSA. We’ve done this to ourselves by allowing the supposed government regulators ‘protecting’ us to NOT do their jobs.